Top ZO Skin Health Products You Need to Try: Exfoliating Polish, Growth Factor Serum & More
Imagine waking up each morning to glowing, refreshed skin — the kind that feels like it belongs in a luxury skincare commercial. That’s exactly what ZO Skin Health aims to deliver. Founded by world-renowned dermatologist Dr. Zein Obagi, ZO Skin Health has earned a loyal following by combining science-backed formulations with real-world results.
But with so many options out there, where should you start? Today, we’ll explore the top ZO Skin Health products that are truly worth the hype, including their cult-favorite Exfoliating Polish and the transformative Growth Factor Serum.
Why ZO Skin Health Is a Game-Changer in Skincare
If you’ve browsed beauty shelves lately, you’ve probably noticed a surge in professional-grade skincare brands. They stand out because they bridge the gap between therapeutic treatments and everyday skincare. Their products are crafted to restore skin health at a cellular level, targeting concerns like aging, pigmentation, and sensitivity — not just covering them up.
ZO Health Skin Care isn’t just about looking good; it’s about achieving skin that genuinely functions at its best.
Must-Try Products From ZO Skin Health
1. ZO Skin Health Exfoliating Polish
One of the brand’s most raved-about products, the ZO Skin Health Exfoliating Polish, is a spa day in a jar.
Infused with ultra-fine magnesium crystals, it gently sloughs away dead skin cells, leaving your skin baby-soft and radiant. Regular use helps unclog pores, reduce dullness, and even smooth out rough texture — all without feeling harsh or irritating.
Pro Tip: Use it 2–3 times per week for best results and follow with a hydrating serum to lock in moisture.
2. ZO Skin Health Growth Factor Serum
Next on the must-have list is the ZO Skin Health Growth Factor Serum. Think of this as your skin’s personal trainer. This lightweight, silky formula boosts elasticity, improves firmness, and reduces the appearance of fine lines.
It’s packed with clinically proven growth factors that stimulate your skin’s natural repair process, making it a favorite for anyone looking to combat early signs of aging without heavy or greasy creams.
Pro Tip: Apply it at night for a powerhouse overnight rejuvenation.
What Are People Saying? A Look at ZO Skin Health Reviews
ZO Skin Health reviews consistently highlight noticeable improvements in texture, tone, and hydration. Many users share stories of how these products helped restore their confidence after years of battling uneven skin tone, acne scars, or dryness.
Of course, every skin journey is unique. But the overwhelming positivity speaks volumes about how Health Skin Care products deliver results when used consistently and properly.
More Worthy Mentions from ZO Skin Health
While the Exfoliating Polish and Growth Factor Serum steal the spotlight, there are plenty of other gems in the ZO lineup. Some fan favorites include:
- Daily Power Defense: A potent antioxidant serum that shields your skin from environmental stressors.
- Complexion Renewal Pads: Perfect for keeping oily skin in check throughout the day.
- Smart Tone Broad Spectrum SPF 50: A sunscreen that adapts to your skin tone and provides excellent protection without a chalky finish.
How to Start Your ZO Health Skin Care Routine
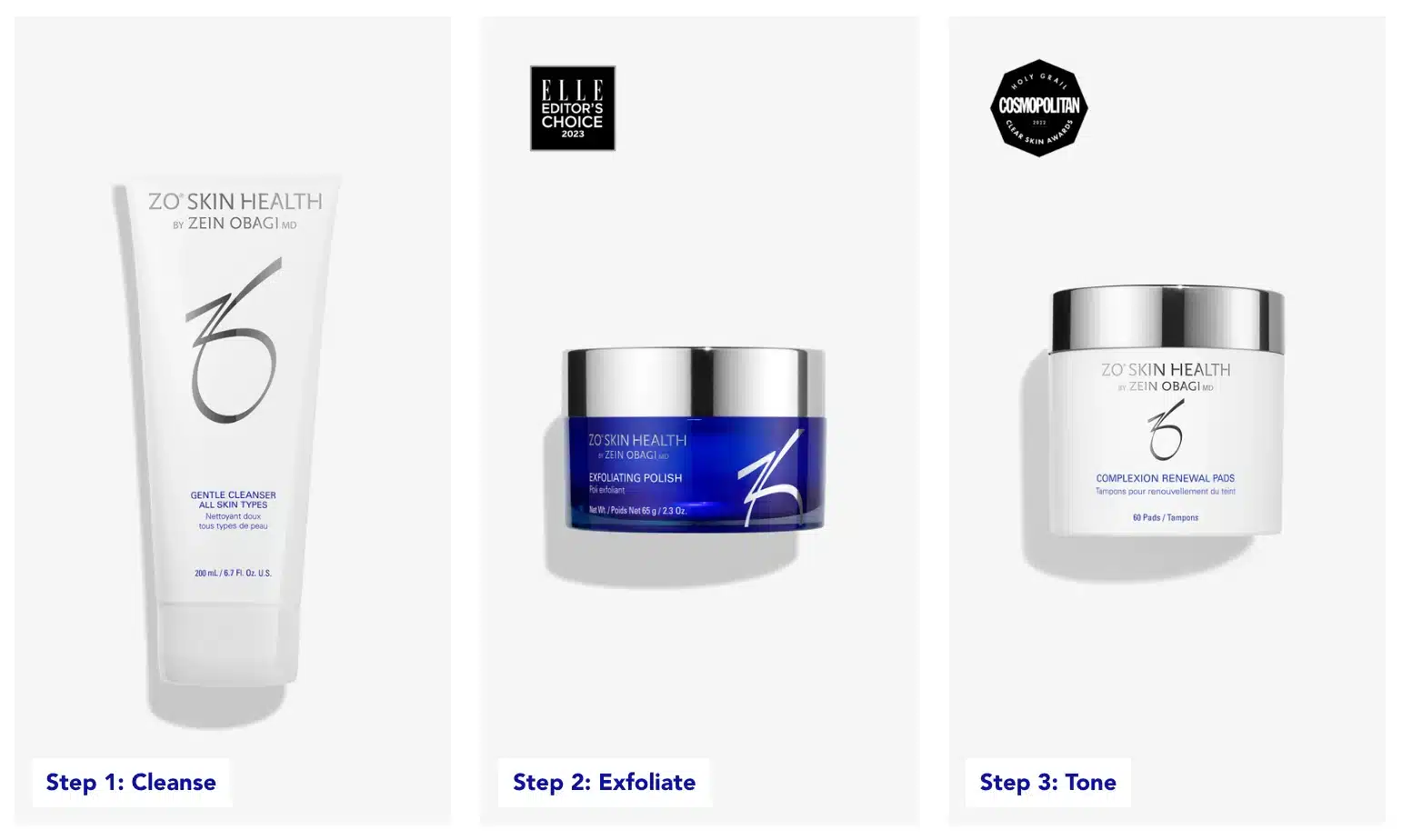
If you’re new to ZO products, it’s best to start with a simple routine:
- Cleanse ➔ Exfoliate ➔ Correct ➔ Protect.
You can gradually introduce more specialized treatments based on your skin’s needs. And don’t forget — consistency is key!
If you’re unsure where to start, consulting a ZO Skin Health specialist can help tailor a regimen perfect for you.
Investing in your Skin
When it comes to investing in your skin, quality matters. ZO Skin Health offers a professional-grade line that’s trusted by dermatologists and loved by skincare enthusiasts worldwide. Whether you’re looking for a brighter complexion, firmer skin, or an all-around healthy glow, adding staples like the ZO Skin Health Exfoliating Polish and ZO Skin Health Growth Factor Serum could be the game-changer your routine needs.
Ready to unlock your skin’s potential? Maybe it’s time to give ZO Health Skin Care a try!
FAQs
ZO Skin Health combines therapeutic-grade ingredients with cutting-edge technology to treat the skin at a cellular level rather than just the surface.
For most skin types, using the Exfoliating Polish 2–3 times a week is sufficient to maintain a bright, smooth complexion.
Users often report improved skin elasticity, reduced fine lines, and an overall healthier, firmer skin texture within a few weeks.
Some products are formulated for sensitive skin, but it’s best to consult with a skincare professional before starting any new regimen if you have sensitivities.
You can purchase them through authorized medical practices or directly from the official ZO Skin Health website.






